IVF Treatment
With the advancement of modern science in the last few decades, assisted reproduction has become a successful and common course of treatment for infertile individuals and couples. In-Vitro Fertilization, IVF, is one such assisted reproductive technique that has been employed successfully as a solution to a range of infertility issues. The IVF process is both safe and effective, and it has been used in the early 1980's in helping infertile individuals and couples achieve their goal of becoming parents.
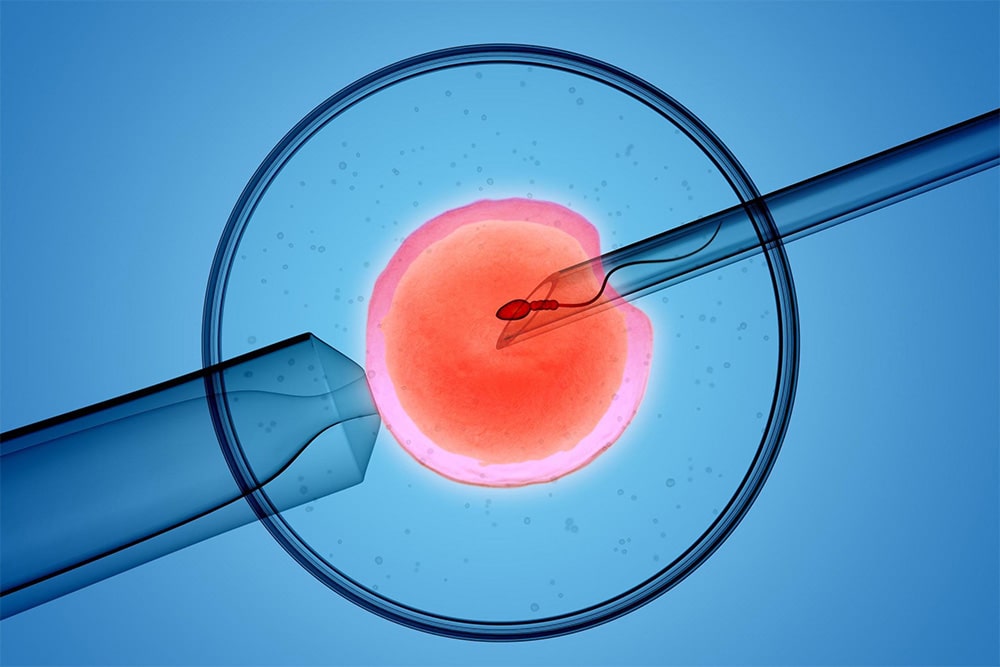
In vitro is Latin, meaning "in glass," referring to the dish that is used to introduce the sperm to an egg. The term "IVF" includes a whole spectrum of assisted reproductive treatment possibilities that can be used separately or together to increase the chances of success. Whenever possible, IVF is used to fertilize an egg with a sperm, thereby forming an embryo
Fertility treatment often includes use of hormone therapy to stimulate the ovaries to produce eggs. Then, IVF begins with retrieval of a woman's (or her donor's) eggs. Prior to the retrieval of the eggs, the male partner (or a donor) produces a semen sample, which is processed and washed, and the most motile (active) sperm are selected. Anywhere from three or four, or even up to twenty eggs are retrieved from the woman under general sedation. This procedure requires no surgical incision and is done purely on an outpatient basis in our office. The retrieved eggs are placed in a separate dish under a protective layer of oil and left alone for three to four hours to complete their maturation.
There are two options are available in the lab. The first is routine IVF, where the washed sperm is added in a measured quantity to each dish containing an egg. This method requires numerous amounts of motile sperm from the male. The second is ICSI, which is recommended when either the quality or the quantity of sperm is low. ICSI is also useful when the zona pellucida – the membrane surrounding the egg – is so thick that the sperm cannot penetrate on its own and requires forced injection. Done under a high-powered microscope, ICSI involves selecting one sperm and injecting it into an egg. Both IVF and ICSI procedures are carried out by the well experienced in house embryologist, who is a back bone of an ART center.
What are the risks of IUI?
The main risk for IUI is the risk of multiple gestations, especially of high-order multiples (triplets or more). This is an inherent risk that is extremely difficult to avoid. The difficulty lies in the fact that the physician does not have good control over how many eggs are released at the time of ovulation, and how many of those eggs are fertilized by the semen from the IUI. Physicians try to strike the right balance between good pregnancy chance and a low risk for multiple gestations, but even in best of hands, high-order multiples will happen.
Fertility practice has come to try to avoid multiple births, especially high-order multiples, because they carry elevated risks, especially of premature delivery. The goal of good infertility treatment is, of course, not only to achieve pregnancy but to achieve pregnancy responsibly, and with as low risk as possible to mother and newborn children.
Day 1: Check for Fertilization
About 16-18 hours later, the embryologist inspects the eggs under a microscope to ascertain whether they have been fertilized – whether the sperm has successfully penetrated the egg to create an embryo. The embryologist does so by looking for specific formed signs or genetic (pro-nuclear) changes: when a sperm enters an egg, it "wakes up" the condensed genetic material of the egg, activating or "opening" it and beginning the process of growth. The number of eggs fertilized is thereby noted. This is the earliest stage at which embryos can be frozen. Elective freezing enables the preservation of a woman's potential fertility well past the time when her body could hypothetically stop producing viable eggs.
Day 2: Monitor Growth
The fertilized eggs – embryos – are monitored in the lab as they begin the process of division. Within the next 24 hours a single embryo divides one or two times into a two-celled or four-celled embryo.In some indicated patient our doctors would consider to do the embryo transfer on day two of embryo growth.
Day 3: Monitoring of Embryo Development
Over the following 24 hours, the embryo, which has divided further into either four or eight cells, can now be transferred to the uterus. Alternatively, the divided embryos can be frozen at this stage for the preservation of future fertility. Also, the divided embryos can grow for a further 48 hours to the blastocyst stage, where either a transfer or freeze cycle can be accomplished (blastocyst transfer is explained below).
Day 3: Assisted Hatching
Another technique used at our centre to increase a woman's chances of implantation is assisted hatching. To successfully implant in the womb, the outer layer or "shell" of the embryo, called the zona pellucida, must break, allowing the embryo to "hatch out" and attach to the endometrial lining. However, as a woman ages, her eggs may develop thicker shells, making it more difficult for the egg to hatch naturally; or, the embryologist may have Identified as a poor embryos from a previous IVF cycle. In these scenarios, the Embryologist may choose to employ assisted hatching, which is the process by which a hole is created in the shell of the developing embryo, using mechanical or chemical means, to facilitate the natural process of hatching and improve the chances of implantation with embryo-transfer.
Day 3: Preimplantation Genetic Diagnosis
Day 3 is also the time when advanced techniques such as preimplantation genetic diagnosis are carried out. This technique employs molecular genetic methods to enable the identification of genetically normal embryo.
Day 5-6: Blastocyst Transfer
If it is decided that blastocyst transfer may be more successful for a particular patient, instead of the initial day 3 transfer, the lab will allow a fertilized embryo to multiply for 5-6 days in the dish, growing to the blastocyst stage.
The blastocyst is an advance-developed embryo, consisting of the inner cells (the developing embryo) in a fluid-filled cavity, all encased in the outer layer that will later become the placenta. In a natural pregnancy, this is the stage where the embryo—which would have been traveling down the fallopian tube—would implant in the womb. Transferring to the uterus at this stage is called a "blastocyst transfer."
How IVF Works?
One of the great advantages of IVF is that it can treat many causes of infertility. These conditions include, tubal blockage, problems with ovulation, problems with the way the sperm and egg interact, poor sperm quality or quantity, older patients, problems with the cervix and many more.
Another great advantage of IVF is that it can be used to make specific diagnosis. Since the embryo is created in the lab it gives specialist the ability to test the embryos for any genetic or chromosomal problems. IVF therefore can be used to diagnose inheritable diseases. Some of the most common diseases tested are cystic fibrosis, sickle cell disease, and chromosomal problems such as Downs's syndrome and Turner's syndrome.
Who needs IVF?
At Santhathi Fertility Centers it is our mission and goal to treat our patients based on their diagnosis and the most efficient and cost effective way to achieve the goal of pregnancy. Not everyone needs IVF. IVF is perhaps the best way to treat infertility. Depending on the cause of infertility IVF may be the first-line of treatment. IVF in other cases is recommended when more conservative treatment options fail.